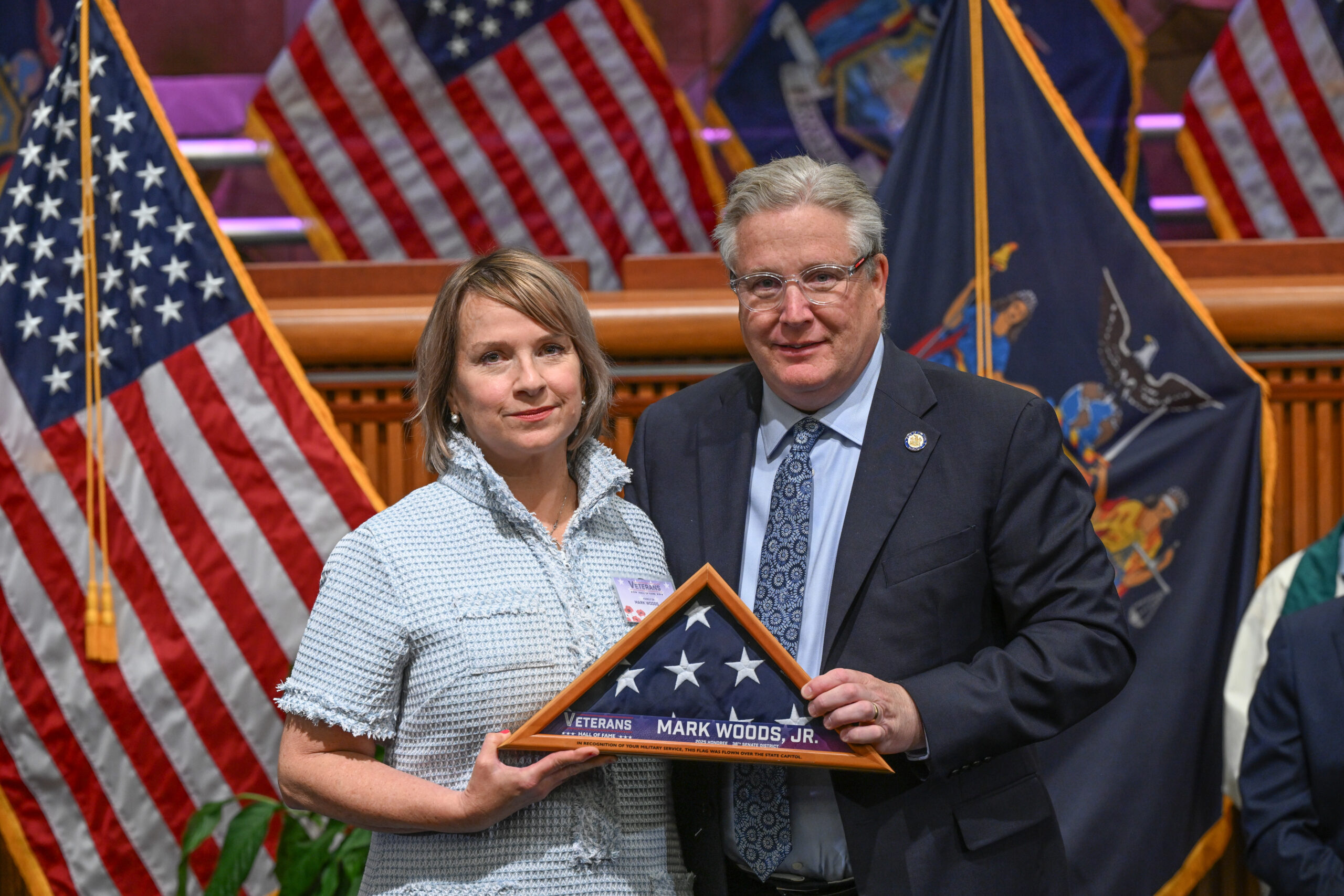
ROCKLAND COUNTY, NY – This week, State Senator Bill Weber posthumously inducted Town of Clarkstown Councilman Mark Woods Jr. into the New York State Senate Veterans Hall of Fame in a ceremony held at the State Capitol.
Mark’s beloved wife, Jeanne, his daughter, Maggie, his son, Ray, and his mother, Marie, joined the ceremony to accept the award on Mark’s behalf.
A Brooklyn native, Woods was commissioned as a Second Lieutenant in the U.S. Army Infantry after attending The Citadel. He served in Berlin at the end of the Cold War and deployed to Bosnia for peacekeeping operations. His civilian career included service as a corrections officer, border agent, and NYPD officer, where he was part of the Vice Squad and the Joint Terrorism Task Force. He returned to active duty in Iraq post-9/11 before continuing his public service stateside.
Woods later became Deputy Director of the Rockland County Veterans Service Agency and then Director of the Joseph P. Dwyer Veterans Peer Support Program at BRIDGES, where he supported fellow veterans through mental health and crisis recovery work. His advocacy and compassion touched countless lives.

“Mark Woods Jr. exemplified the spirit of selfless service,” said Senator Weber. “His dedication to his country, his community, and especially to his fellow veterans, was unparalleled. This induction ensures that his legacy of compassion, leadership, and service will be remembered and honored for generations to come.”
“I can think of no one more deserving at this moment. Mark Woods is the purest example of a serviceman dedicated to his country and his community. He was humble, passionate and undeniably committed to seeing our community be better. I can’t think of a better way to pay tribute to a selfless man like Mark Woods and his enduring legacy than his induction to the NYS Veterans Hall of Fame.” said Carlos Martinez, LMSW, CEO and Executive Director of BRIDGES
Clarkstown Supervisor George Hoehmann, a good friend of Mark Woods added, “I am proud to help honor the life and legacy of Mark Woods. From his service in the U.S. Army to the streets of NYC as an NYPD officer, to his compassionate work with our veterans and as Town Councilman, his unwavering commitment to helping others will always be an inspiration. Clarkstown and New York State will never forget his lifetime of service.”
The New York State Senate Veterans Hall of Fame honors the courage, sacrifice, and service of veterans who enrich their communities long after leaving active duty. Mark Woods Jr. stands among the finest examples of that enduring legacy.


 Police/Fire/EMS1 week ago
Police/Fire/EMS1 week ago
 Community1 week ago
Community1 week ago
 Politics1 week ago
Politics1 week ago
 Government1 week ago
Government1 week ago